Complexity theory is pretty sexy in implementation research right now. Like, Ian Malcolm in the first Jurassic Park talking about chaos and strange attractors kind of sexy. I must confess however to originally having some scepticism. It’s all very well talking about how “complex” the system is, but what does that mean in practice? What do we do with that knowledge?
Fortunately, this does seem to be moving on. More recent papers actually talk about the implications of this for how we work, what it looks like in reality to “embrace complexity” and how this is different to business as usual (check out for example SHIFT-Evidence by The CLAHRC North West London team, or the recent BMJ paper on complexity and improvement by Jeffrey Braithwaite.)

You’re welcome.
Nevertheless, a lot of it is still described in somewhat impenetrable academic-speak. Fractals, non-linear dynamics, emergent properties etc etc. To be fair, these are publications from academic journals so the academic speak is appropriate there. In the spirit of making theory more accessible though, I wanted to break it down, and also to think about what *doing* a complexity approach means in health research.
So, what does complexity theory really mean? I’ve boiled it down to 4 actions. Talk, Tailor, Test, and Track.
Talk
Lots of the complexity papers describe health as ‘a living system’. It has People in it, and there’s nowt as queer as folk. They tend to have their own opinions. They have burdensome histories, they have urgent presents, they have desired futures. They sometimes don’t do what we want. They almost never do what we expect. How do we tackle that? We talk. And we listen.
People react to things, especially New Things that we’ve dropped on them. We need to understand that they are ‘active mechanisms’ (in academic speak) in what happens – how they react will be crucial to whether our shiny New Thing works or fails.

Your shiny New Thing might not actually be what people think they fit best.
Their environments are complex. There are ‘hidden variables’ (academic speak), meaning stuff going on that you might not know about if you only take a top-level view. The way things are actually done might not look much like the tidy flow chart that the chief exec has on their wall. If you only plan to intervene based on the flow chart, then you’re probably going to have a shock.
There are more academic ways of trying to understand this such as ethnographic observation and soft system modelling. But, in the interests of simplicity, probably the most obvious way to get to grips with this is to have a conversation. We talk.
So, now we (hopefully) understand our “living system” a bit better. We have a sense of what really happens, and what people really think. But now what? How do we use that to try to improve our projects?
We Tailor.
Tailoring means acknowledging that “one size does not fit all”. It’s about matching our New Thing to what the people there want or need, or fitting our New Thing better to how things are actually done on the ground. This might be mean adapting how something is done locally, so it fits with their workflows and resources. It might mean framing the project itself so it matches with their priorities, or helps them meet a new national directive. At it’s core, this is about understanding that the ‘research to practice gap’ is less about research jumping over a gulf than it is about research not fitting into spaces that exist in practice.
This is about recognising that local diversity is not noise to be analysed out but part of if and how something works, and if we continue to neglect it, we will continue to have stuff that doesn’t work. A colleague of mine described this perfectly as “no more drag and drop interventions”.
It’s important to acknowledge that there is a tension here between tailoring and the traditional research aims of replication, standardisation, and generalisability. In research we typically want things to be The Same everywhere, both for purity in our testing approaches and because this then makes it easier to roll out (if it’s found in those tests to be effective). If it’s not the same, then how do you efficiently scale up something that is different everywhere? Personally I think there’s a fascinating space here to explore how we can identify and work with the core ingredients of a New Thing (which would be The Same, and delivered and tested everywhere) but also map out where this is potential for adaptation. This would put the pressure on us to define exactly what works in our New Thing (what are the core features that are essential to making something happen) but also how it works – what are the fundmental mechanisms that are at work, even if they are put into action in different ways? How are these activated in specific contexts, and who does this?

We need to identify and report what should look the same, and what’s different…
So, we talked (and listened) and we tailored. Now we just get stuck in and deliver, right? Not quite…
We Test. Yes, we now run something and check the effect. But, if you’re a complexity type , you think it’s better to start this small to begin with, and it’s better to do this repeatedly. Think feedback loops and iterative learning (this is where learning health systems fit in). This stage acknowledges that any amount of talking can’t beat a live run, and you learn a huge amount about what works and what doesn’t. Things Will Go Wrong. This is fine, if we’ve made space in our projects to learn from this. I’ve known of trials where it became obvious very early on that the intervention wasn’t being delivered, because it turned out people couldn’t do it properly, or the context changed (see below). But the trial still trundles on. This is arguably an enormous (and unethical) waste of time and money. This is why local testing, on the ground, with the users, is so essential. Fail faster, as the adage goes.
Ok, ok, we did all that. Now we just do it, right? Almost…
Now, we Track.
The key thing now is that things change over time (emergent properties in academic speak). There’s a paper by Carl May and colleagues that explains this really nicely: context is not just a where, but a when. Changes can be surprises – staff can leave, new leadership comes in, competing priorities or directives emerge, funding gets cut. Or they can be deliberate – local adaptations (such as the ‘tinkering’ that iPARIHS talks about), for example through the iterations you’ve undertaken in the “test” stage. They can be both deliberate and surprising for the research team, as when users ‘game the system’ or hack what we wanted them to do to do something else. These are our ‘non-linear dynamics’ which is a fancy academic way of saying “blimey, we never thought that would happen”.
Fundamentally, we need to treat time as a variable, and change as a mechanism of action rather than a deviation from course. We need to understand implementation as a process rather than a thing. Longitudinal data collection is our friend here.
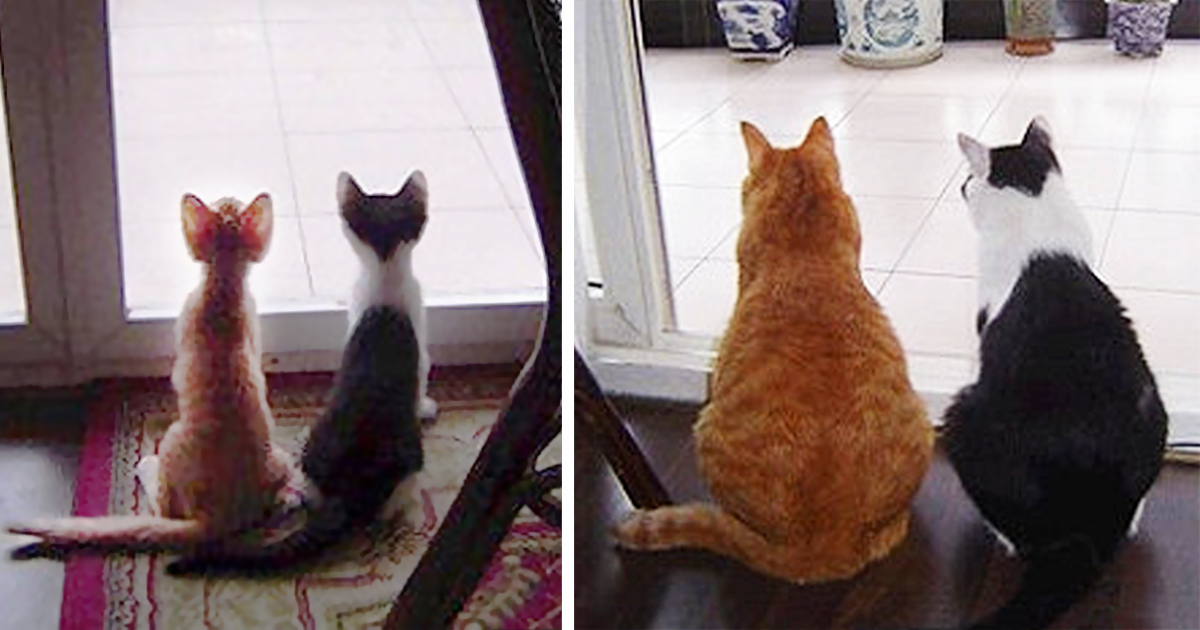
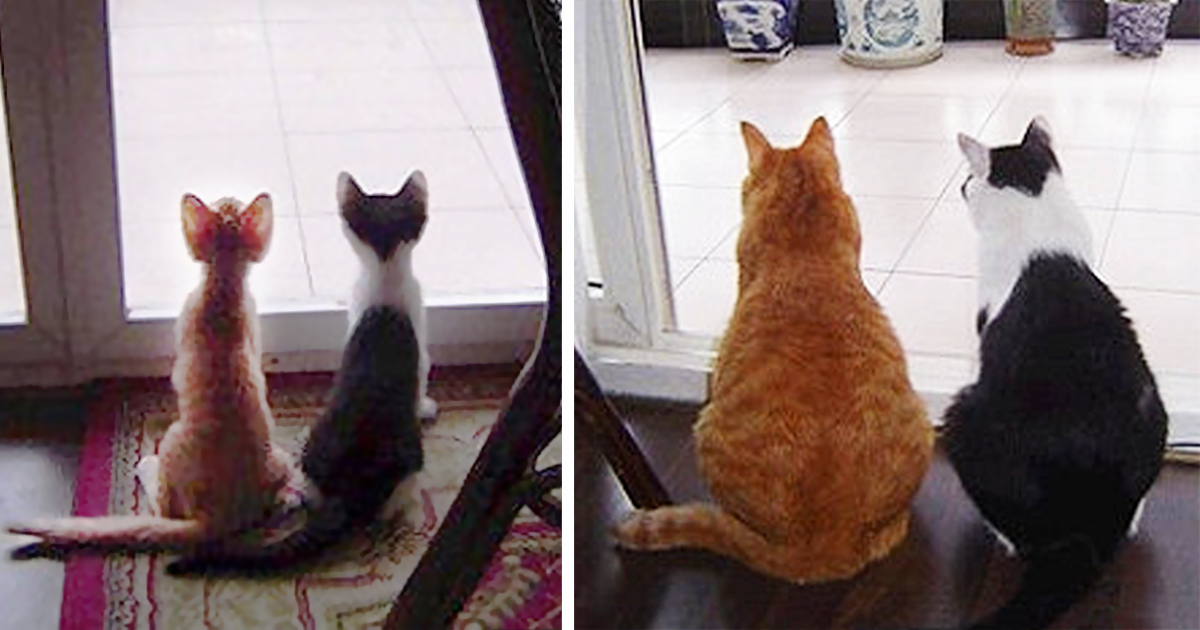
Things look different over time…
So there we go. Much of the above is of course simplified, and there’s a lot more that complexity theory adds, or challenges, about health services research and implementation, and there are certainly challenges for complexity approaches too (the best ways of achieving these things in practice and how to adequately report and evaluate them) Nevertheless, I think these are the actionable and hopefully sensible take-aways for implementing New Things.
What do you reckon? Are they surprising, or obvious? Do they help? Let me know in the comments or on twitter.
PS. We have a paper that explores the implications of these things for an “intervention”approach to health research. How we do we include the Talking, how do we acknowledge change? You get messy.